Atrial fibrillation (AF), commonly known as AFib, is a common cardiac arrhythmia characterized by the loss of regular, organized electrical activity in the atria, replaced by rapid and irregular fibrillation waves. It is a serious disorder of atrial electrical activity. AF typically presents as an irregular and fast heart rate, caused by the atria losing their normal rhythm.
【Etiology】
1. Structural Heart Disease
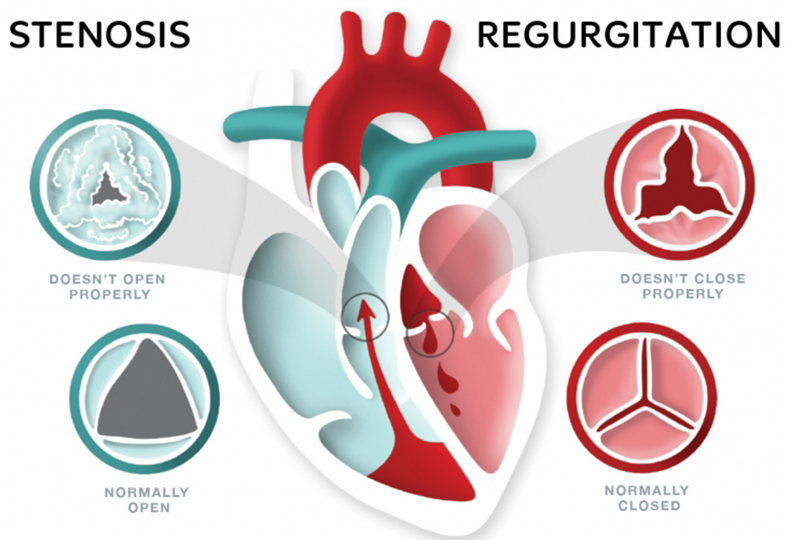
(1)Rheumatic heart disease: accounts for about 33.7% of the causes of atrial fibrillation, with mitral valve stenosis and insufficiency being common.
(2) Coronary heart disease: confirmed by coronary angiography, the incidence of atrial fibrillation is 1.5% in patients with angina pectoris, 3.8% in patients with old myocardial infarction, and 8.2% in patients with acute myocardial infarction. In patients with chest pain who have normal coronary arteries confirmed by coronary angiography, the incidence of atrial fibrillation is 11%. In general, the incidence of coronary heart disease is relatively low.
(3)Hypertensive heart disease: many small arteries of the atrial muscle can narrow or completely occlude due to intimal thickening, leading to ischemic changes and fibrosis in the local myocardium.
(4)Hyperthyroidism: early myocardial focal necrosis and lymphocytic infiltration, with long-term cases often showing fine, localized fibrosis, with an incidence of 5%, more common in patients aged 40 to 45. It is less common in young patients and, if it occurs, is often paroxysmal.
(5)Sick sinus syndrome: when there is local developmental dysplasia of the sinoatrial node arteries, abnormal collagen structure, and degeneration around the sinoatrial node, especially degeneration around the sinoatrial node and abnormal sinoatrial impulse, atrial fibrillation can occur.
(6)Cardiomyopathy: all types of cardiomyopathy often lead to atrial fibrillation due to focal myocardial inflammation, degeneration, or fibrosis, as well as atrial enlargement predisposing to atrial fibrillation. Atrial fibrillation in alcoholic cardiomyopathy patients is often the first manifestation of the disease, with a high incidence.
(7)Other heart diseases: such as pulmonary heart disease (with an incidence of 4% to 5%, mostly paroxysmal, and the attacks decrease after improvement in respiratory function); chronic constrictive pericarditis; congenital heart disease, etc. Atrial fibrillation is characterized by increased focal origin automaticity; some paroxysmal, persistent, and chronic atrial fibrillation is caused by local micro-reentrant mechanisms in the atrium, pulmonary veins, and vena cava.
2. Preexcitation Syndrome
Preexcitation syndrome may occur due to a short refractory period of the accessory pathway in patients. Once the conditions for reentry are established, the impulse increases through the bypass pathway. This impulse can then reenter the left atrium during its refractory period, triggering atrial fibrillation. The incidence of atrial fibrillation complicating preexcitation syndrome is 11.5% to 39%. Atrial fibrillation complicating preexcitation syndrome is considered serious because the bypass pathway does not have the protective effect of physiological conduction delay like the atrioventricular node. Therefore, the ventricular rate conducted through the bypass is often above 180 beats per minute, severely affecting the heart's pumping efficiency.
3. Other diseases
(1)Systemic infiltrative diseases such as systemic lupus erythematosus, scleroderma, leukemia, amyloidosis, etc.
(2)Pulmonary and systemic infections, as well as chronic pulmonary insufficiency.
(3)Heart surgery and trauma.
(4)Digitalis toxicity, aconitine alkaloids, nicotine poisoning, etc., can all induce atrial fibrillation.
(5)Various cardiac catheter operations and procedures such as esophageal electrostimulation, electrical cardioversion, etc., can directly induce atrial fibrillation.
(6)Excessive alcohol consumption, smoking, emotional stress, excessive smoking, urination, etc., can directly cause or induce atrial fibrillation on the basis of existing heart disease.
4. Familial Atrial Fibrillation
It is caused by genetic mutations and is inherited in an autosomal dominant manner. It often occurs after adulthood, presents as paroxysmal, and occurs and terminates without being noticed. The symptoms of atrial fibrillation are mild, mostly induced by fatigue, mental stress, infection, pain, alcohol consumption, smoking, etc., and the heart function remains normal. The prognosis is generally good.
5. Unknown reasons
Idiopathic atrial fibrillation that occurs in healthy individuals often lacks evidence of structural heart disease.
【Clinical Manifestations】
1. A few patients may have no obvious symptoms, or only palpitations, chest tightness, and anxiety.
2. Some severe cases may present with dizziness, syncope, angina pectoris, acute heart failure, or even acute pulmonary edema.
3. Some patients may experience systemic arterial embolism, with cerebral embolism (stroke) being the most common.
4. The ventricular rate is fast and irregular, usually between 120 and 180 beats per minute. The rhythm is absolutely irregular, the intensity of heart sounds varies, and there may be pulse deficit (pulse rate less than heart rate). When the ventricular rate is below 90 beats per minute or above 150 beats per minute, the irregularity of the rhythm may not be obvious.
【Examinations】
Examinations may reveal signs suggestive of atrial fibrillation. Electrocardiography is valuable for diagnosis, and echocardiography is helpful for identifying the etiology and understanding the prognosis. Most patients with atrial fibrillation may experience discomfort such as palpitations or chest tightness, making routine physical examination crucial. Atrial fibrillation can be divided into three stages: early paroxysmal (atrial fibrillation can stop spontaneously), middle persistent (atrial fibrillation can be stopped by medication, etc.), and late permanent (atrial fibrillation cannot be stopped).
【Differential Diagnosis】
1.Differentiation between atrial fibrillation with intra-atrial conduction delay and ventricular premature beats.
2.Differentiation between atrial fibrillation with intra-atrial conduction delay and ventricular tachycardia.
3.Differentiation between preexcitation syndrome with atrial fibrillation and ventricular tachycardia.
4.Differentiation between atrial fibrillation and atrioventricular nodal rhythm.
【Treatment】
1.Principles of treatment: Eliminate predisposing factors; restore and maintain sinus rhythm; prevent recurrence; control ventricular rate; prevent complications of embolism.
2.Drug therapy: Antiarrhythmic drugs, anticoagulants.
3.Electrical therapy: Electrical cardioversion, artificial cardiac pacemaker, catheter radiofrequency ablation.
4.Surgical treatment: Surgical maze procedure.











 沪公网安备 31011502014876号
沪公网安备 31011502014876号 are registered trademarks of MicroPort CardioFlow Medtech Corporation.
are registered trademarks of MicroPort CardioFlow Medtech Corporation.